Physiological
Resuscitation: Placental Transfusion
Many physiological factors control and effect the transition
from placental life support to independent life support – resuscitation. [1]
1.
The “cold crying reflex.” Cool air on wet skin.
2.
Lung aeration
dilates pulmonary arterioles.
3.
The
“cold pressor reflex” increases systemic blood pressure reversing Ductus A.
flow.
4.
Massive
placental transfusion initiates the pulmonary circulation.
5.
Pulmonary
blood flow “erects” alveoli – the “Jaykka” effect. [2]
6.
Pulmonary
blood flow closes the foramen ovale.
7.
Oxygenated
blood flow closes umbilical arteries
8.
Oxygenated
blood flow closes the D. A.
9.
Increased
central venous pressure from placental transfusion reflexively closes all
umbilical vessels in the abdomen and the ductus venosus. [3]
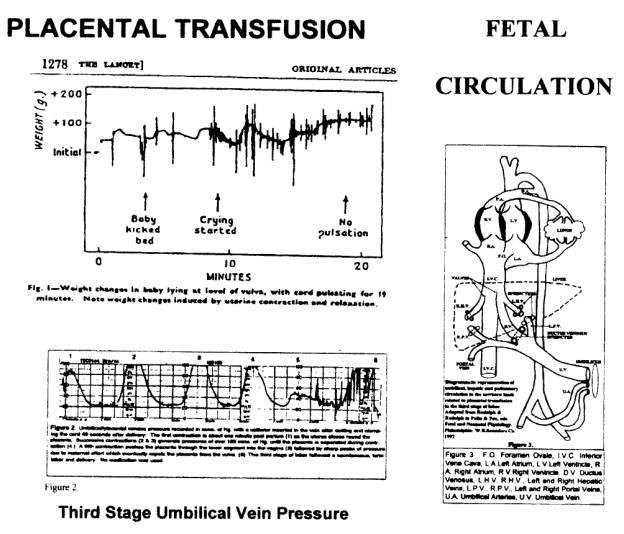
In Gunther’s Figure 1, [1] the child was wrapped in a warm
blanket and placed on a scales at the level of the vulva. Without a “cold” stimulus for crying,
placental respiration continued for nearly ten minutes. Gravity did not influence placental
transfusion that was effected purely by uterine contraction.
At the ten-minute mark, the child received about 100mls of
blood transfusion within 30 seconds at considerable hydrostatic pressure.
The recording of umbilical venous pressure [UVP] was generated by the post partum uterus against a
closed cord. It indicates that the
child’s (Figure 1 [1]) vena cava, heart, great vessels and lungs were distended
at pressures exceeding 100mms Hg. producing a marked “Jaykka” [2] effect.
Gunther notes that crying often occurred at the peak of a
transfusion, possibly the result of painful liver distension. [1]
The “step and plateau” pattern of the final minutes
indicates reflexive sphincteric closure of the vessels, with the vein sphincter
acting as a pressure valve, preventing blood loss and excess transfusion. Until this reflex is activated, crying may
increase blood loss.
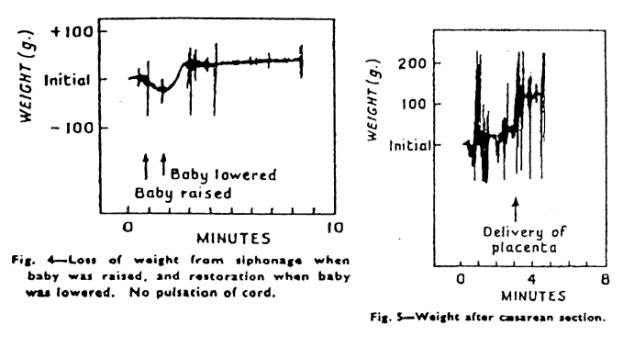
Other newborn weight tracings in Gunther’s paper show blood
loss and blood transfusion caused by gravity – placing the child above or below
the placenta. At the typical birth when
a child cries soon after delivery, the pattern of transfusion is similar to the
last five or ten minutes of Figure 1. [1]
Major hemodynamic changes occur following placental
transfusion. Immediately after
physiological cord closure central venous pressure may be as high as 10 mms Hg.
[3] Blood volume is reduced by hemoconcentration as the higher systemic blood
pressure forces fluid into the extracellular space. There is a corresponding
increase in blood albumin concentration and the increased colloid osmotic
pressure ensures that pulmonary edema does not occur, and any alveolar fluid is
readily absorbed.
Increased
blood pressure increases kidney glomerular filtration and urine output is
copious, excreting the excess interstitial fluid produced by hemoconcentration.
Thus physiological cord closure produces a physiological
(healthy) neonate with a normal blood volume.
Not only is placental respiration maintained until pulmonary respiration
is established, but all other life support systems (gut, kidneys, brain,
respiratory muscles) of the child are activated by means of placental
transfusion and the fetal circulation is converted to the adult.
Reference:
1.
Gunther
M. The transfer of blood between the baby and the placenta. Lancet 1957;I:1277-1280.
2.
Jaykka S. Capillary
Erection and Lung Expansion. Acta
Paediatr. 1965 [nppl] 109
3.
Arcilla RA, Oh W. Lind J.
et al. Portal and atrial pressures in the newborn period. Acta Paediatr. Scand. 1966;55: 615-625
www.cordclamp.com Neonatal Resuscitation: Life that Failed.
Copyright September 2004 G. M. Morley MB ChB FACOG