Hypoxia / Asphyxia Treated with
Placental Transfusion
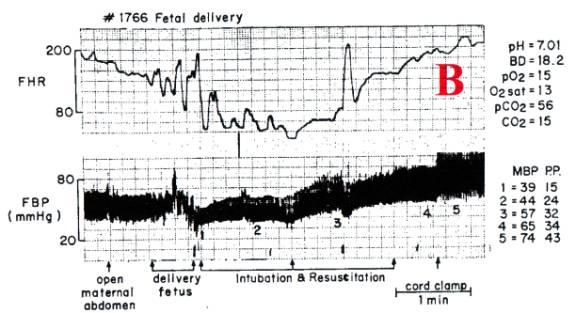
The tracing [B] shows
the effect of pure anoxia combined with delayed cord clamping. This primate’s mother was breathing pure
nitrogen. The bradycardia caused by
hypoxia and decreased cardiac output is noted, but delivery and resuscitation
were done before the heart failed – there was some decline in blood pressure
(depression of cardiac function) at birth, but no steady decline to zero as in
[A]. RR
did not occur.
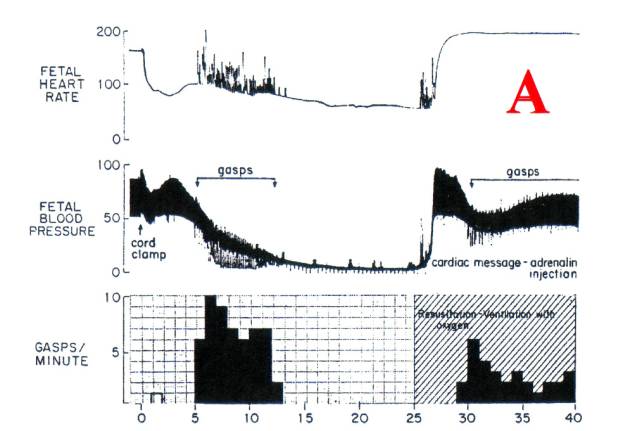
The results of resuscitation are strikingly different
in these cases. In [B], BP increases steadily as the lungs (and the
neonate) fill with placental transfusion; following cord clamping there is a
dramatic rise in BP. In [A], after the resuscitation adrenaline effect is over,
the blood pressure / cardiac output fall to levels that again stimulate
gasping. Note the effect of
immediate cord clamping on the [A] heart rate
– a precipitous fall; such an accident occurring during labor would precipitate
a crash c-section. This primate’s
placental transfusion was clamped in its placenta [A]
at birth. Resuscitation filled the
lungs with oxygen, but pulmonary blood volume was withdrawn from the systemic
circulation, leading to hypovolemia, hypotension and gasping.
Primate
[A] was severely brain damaged (before
resuscitation). Primate [B] was normal.
DOES IT
REALLY WORK?
EMAIL: Hi Dr. Morley, I just did a birth yesterday
that was a perfect example of your theory, (one which I have followed for 25
years). I had a 40 year old primip with a long but normal labor and with good
FHR throughout until a sudden drop at crowning, down to 60 with no return
to baseline, after a quick episiotomy and quick birth the baby had already
entered 2nd apnea, I saw it "gasp" before the head was born. The baby
had a nuchal cord as well as a true knot! She came out in a flood of thick
meconium that she had inhaled during her birth. No pulse was palpable at
birth but with the cord intact the pulse quickly came up to normal (APGARS 2,
7, 9) and with a lot of suctioning and her parents touching her and
talking to her and her cord pulsating with a little bag and mask she is fine
and now fully up to "normal" newborn status. When I think back
on how this situation would have been handled in places where I have worked (I
work in an out-of-hospital birth center now) I know this baby would have
ended up in the NICU with mec pneumonia, the cord would have been cut, the
neonatologists would have "saved" the baby, and who knows where the
child would end up years later. Tracy
XXXX C.N.M.
Copyright September 2004 G. M. Morley MB ChB FACOG