Birth-Brain Injury
Caused by Umbilical Cord Clamping:
From Imbecility
and Cerebral Palsy to Minimal Mental Retardation
George Malcolm
Morley, MB ChB FACOG
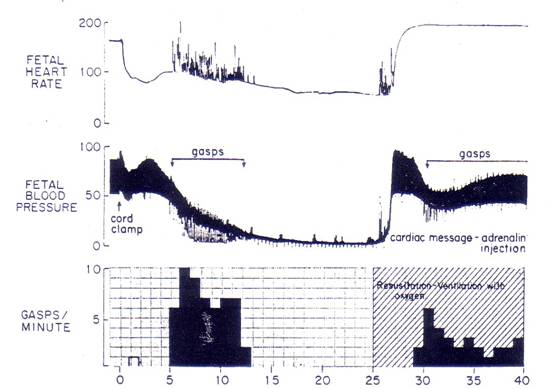
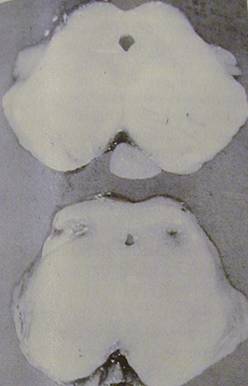
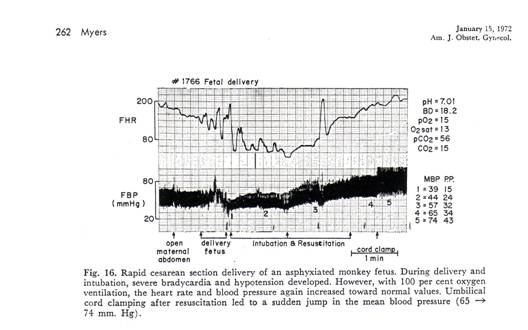
Figure 1 is a
recording of total asphyxiation of a newborn primate delivered by
C-section with electronic monitoring of Fetal Heart Rate, BP and
Respiration. The cord was clamped and
the head placed in a saline-filled bag at birth. Post mortem examination showed massive necrosis
of basal ganglia and the cerebral cortex.
Hypoxia did not injure this neonate’s brain.
Figure 1.
During birth, the VIABILITY of the Central Nervous
System and the myocardium are dependent on perfusion with nutrient blood that
removes the waste products of aerobic and / or anaerobic metabolism. Deficient perfusion will result in tissue
death – infarction – regardless of blood oxygen content.
The FUNCTIONS of the Central Nervous System and the
myocardium (nerve impulses and muscle contraction) are dependent on aerobic
metabolism – OXYGEN. Deficient
oxygen supply results in loss of function. Deficient myocardial function (from ANY
cause) will result in loss of perfusion and tissue infarction.
Cardiac arrest (no blood pressure for 15 minutes)
infarcted the brain of the above monkey.
Human neonates, born by C-section, are routinely oxygenated within
minutes of birth and never have hypoxic heart failure causing zero blood
pressure. However, the clinical course
of the human newborn that progresses to brain ischemia and brain injury is
often mimicked in the above tracing.
Cerebral palsy
Cerebral Palsy (CP) is only the tip of an enormous iceberg
of birth-brain injury.
The brain damage of CP begins after the baby is born.
The main clinical signs are pallor, apathy, altered tone and difficulty
feeding.
Ischemic
Encephalopathy is diagnosed on MRI, the ischemia is generalized; blood flow
through ALL the brain is deficient, regardless of oxygenation.
Ischemia is the pathogen.
At birth, the basal ganglia and the cortex are growing and
metabolizing actively. In CP, they
undergo ischemic necrosis – infarction.
The
cause of the ischemia is heart failure – failure to generate an adequate blood
pressure – resulting in deficient tissue blood flow.
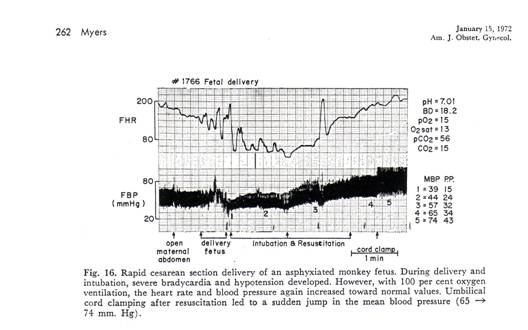
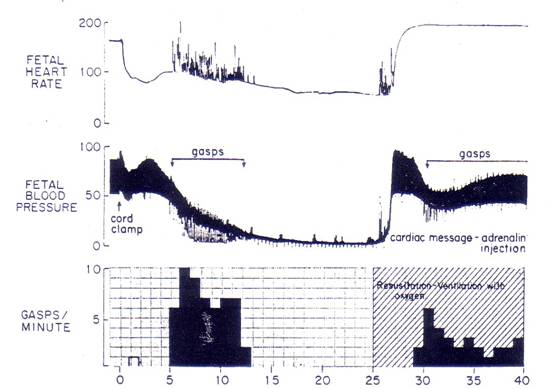
1. Two types of heart
failure are demonstrated in this experiment:
- Anoxic
heart failure.
- Hypovolemic
heart failure – blood loss heart failure.
They have a common symptom – GASPING.
Gasping is retraction respiration, a reflex response to
heart failure – a response to critically low BP and very low Central Venous
Pressure.
Negative intra-thoracic pressure pulls venous blood into the
lungs and heart, filling the ventricles.
Note the spikes of increased pulse rate as ventricles pump
out blood, but with negligible effect on BP.
Now look at the spikes of diastolic blood pressure down to
ZERO and below ZERO.
Blood is pulled backwards out of low-pressure peripheral
arteries into the thoracic aorta.
Blood flows up and down the carotid arteries, pumped in,
sucked out; very little blood flows through the brain.
Ischemic neuron necrosis probably begins at this point; then
the myocardium fails progressively from anoxia. Ten minutes of cardiac arrest (and brain
damage) follow.
At 25 minutes of asphyxia, resuscitation ventilates the
lungs and oxygenates the blood; blood pressure and pulse rate are well
restored.
Then blood pressure falls and at 50 mms Hg. GASPING
begins again. The heart is oxygenated
and perfect; why is it failing?
Look
at the first action – the cord was clamped. Pulse rate and Cardiac Output
fell 50%: WHY? 50% of venous return to the heart was clamped
off.
50%
of this monkey’s blood volume was clamped in its placenta.
Ventilation then opened the pulmonary circulation that
filled with blood from all other organs – creating systemic blood loss and the
falling BP.
The monkey stabilized with a low blood pressure maintained
by gasping – hypovolemic heart failure.
Remember this scenario.
This degree of anoxia never occurs at human birth, but the
sequence of delivery, immediate cord clamping (ICC), and immediate
resuscitation followed by collapse into pallor, hypotension, and gasping is not
uncommon at human cesarean section. CP
is rare, but large placental blood loss is quite routine.
Term CP babies have a somewhat different case
history; all have an episode of asphyxia during birth.
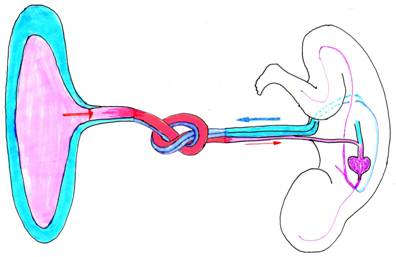
Figure 3. 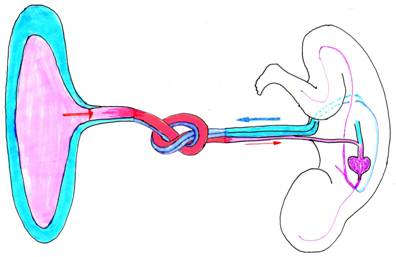
The cause of asphyxia is cord compression – a tight nuchal
cord, a true knot in the cord, a prolapsed cord and/or other cord accident
situations.
The cord vein carries red, oxygenated blood. Compression impedes oxygen flow to the fetus
– hypoxia. As oxygen is dissolved in
blood, compression also impedes blood return to the fetus. Hypoxia entails Hypovolemia.
Net blood flow in cord compression is out of the baby into
the placenta.
The end result is an engorged placenta and a hypoxic,
exsanguinated baby.
These “hypoxic” babies are not born blue; they are ashen
white and dishrag limp; no tone, no reflexes – dead – but with a pulsating
cord.
Rational treatment is to remove the cord compression (loosen
the knot, unwind and release the nuchal cord) and allow oxygenated placental
blood transfusion to restore a normal blood volume and normal oxygenation.
Routine current treatment is immediate cord clamping and
removal to a resuscitation table for immediate ventilation. Think about the resuscitated monkey – it had
some blood volume to fill its lungs.
Little systemic blood is available to fill the lungs of the
cord-compressed newborn.
After ICC, severe hypovolemic shock ensues with retraction
respiration. Ischemic encephalopathy and
CP follow.
PREEMIES have a different scenario.
The most metabolically active part of the preemie’s brain
(and the most vulnerable to ischemia) is the germinal matrix. (GM) It functions from 23 weeks to 36 weeks
gestation. It is extremely vascular with
a copious blood flow; it “boils” out neuroblasts and spongioblasts that migrate
out to grow and form the cerebral cortex.
Immediate cord clamping (ICC) amputates the large placenta
and all its blood; retraction respiration is common; brain ischemia and
infarction of high metabolism areas follow.
Because of extreme vascularity, hemorrhagic infarction of
the G.M. occurs. Bleeding invades
neighboring white matter and the ventricles – IVH – with massive brain
damage. Most cerebral palsy babies are preemies.
Thus the basic ingredients for birth brain
injury are:
- A
metabolically active, growing area of the brain
- Markedly
decreased perfusion of that area caused by
- Decreased
cardiac output / hypotension / hypovolemic heart failure
- Retraction
respiration
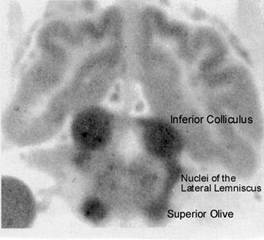
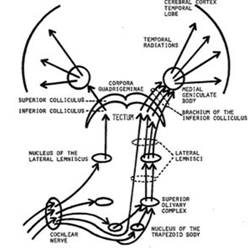
Figure 4. The most
metabolically active parts of the term neonate’s brain are in the nuclei
of the inferior colliculi!
- The
Inferior colliculi are part of the auditory / speech pathway. The defining symptom of autism is
auditory / speech dysfunction – echolalia.
The monkey was neurologically normal, however, its mental
responses were not normal.
When food was placed in one of two containers, and the
monkey released after one minute, it chose correctly 50% of the time. Non-asphyxiated normal monkeys chose
correctly 90+% of the time.
The monkey had very defective recent memory; it could not
pay attention to the food for one minute – it had attention deficit disorder,
ADD.
Many 5-year-old children have ADD, and ADHD, and learning
and behavioral disorders, and autism, ASD and Asperger’s syndrome. They fill special education classes across
the continent. They have a common
denominator – mental deficiency – a low IQ.
If the mid-brain nuclei are as susceptible to ischemic
infarction as are the basal nuclei and the cortex, high-resolution radiography should
demonstrate this in cerebral palsy children, and possibly in autistic children. MRI studies of the inferior colliculi have
never been done on “special education” (SE) children.
As it is, there is plausible proof that many SE children had
severe hypovolemia and brain ischemia during birth – immediate CC and
intra-placental blood loss.
Dozens of studies correlate infant iron deficiency
anemia (during the first year of life) with low IQ in grade school and
learning disabilities.
In
1999, a large study from Dade Co. FL compared infant hemoglobin levels with a
standard IQ test result in grade school:
“The effect of hemoglobin was significant after all
covariates were entered into the equation [odds ratio (OR): 1.28; 95% CI: 1.05,
1.60]. Therefore, for each decrement in hemoglobin, risk of mild or moderate
mental retardation increased by 1.28, even after we controlled for all other
variables in the equation.” (Hurtado)
Normal placental transfusion (no cord clamping) provides
enough hemoglobin and iron to prevent anemia during the first year of life.
Immediate cord clamping causes hypovolemia, hypotension,
ischemia and subsequent infant anemia.
Therefore, for each decrement in hemoglobin, a
corresponding amount of hemoglobin was clamped in the placenta at birth, – with
equivalent increased risk of mental retardation in grade school.
How many newborns are at risk for serious blood loss
during birth, for anemia after birth, and for mental deficiency?
“Sick neonates are one of the most [anemic] heavily transfused groups
of patients in modern medicine.” N A Murray. Neonatal transfusion practice Arch. Dis. Child. 2004
What “group” of patients is prone to blood loss? Mothers have placenta previa and abruption
placenta with massive blood loss, and they also have post partum hemorrhages
that cover the delivery room floor. Four times more newborns
receive blood transfusions than mothers!
ACOG advocated immediate
cord clamping for many years to obtain cord arterial blood pH for medico-legal
documentation. All studies on babies
with cerebral palsy have routine cord pH studies – routine ICC. For many years, every CP baby has had
ICC.
ICC was epidemic in the
1980’s and 1990’s; it still is. ACOG has
withdrawn the Practice Bulletins that advocate ICC, but has not issued any warning
of the known injurious effects of ICC.
C-sections usually have
ICC. C-section babies are 4 times more
likely to be autistic than vaginal deliveries.
Babies from complicated
deliveries are more likely to be autistic than spontaneous deliveries. They routinely have ICC with immediate
transfer to resuscitation.
A recent follow up study
on home births reported zero autism
cases in grade school. In Amish
communities with many midwife deliveries (cord clamping is delayed until the
placenta has delivered), there is no autism epidemic.
But autism is widely
regarded as a genetic inherited trait – many more boys than girls are autistic
– it is surely sex linked. However, when
newborn rats are asphyxiated, then resuscitated, some have no brain damage; most
are female. Most of the neurologically
impaired ones are MALE! Newborn male
rats have a higher metabolic rate than female rats – their brains are more
susceptible to ischemic damage.
The pulse rate of the
average human term male fetus is higher than the female. Male brains are at higher risk of ischemic
damage than female brains.
Admission of women to
college and university is increasing.
For every 100 women receiving bachelor’s degrees, just 73 men get
one. Is this (lower male IQ) the result
of universal ICC over the past 25 years?
1968 William Windle, who
did most of the primate work on brain damage, said this:
9. “A child with a slight
brain defect often appears no different from a normal child. His intelligence
quotient may lie in the range considered normal, but one never knows how much
higher it would have been if his brain had escaped damage in the uterus or
during birth.”
William Windle, 1968
Figure 10.
This monkey was delivered while its mother was asphyxiated in pure
nitrogen. Its cord was not clamped.
The pulse rate and BP
fell with hypoxia, and recovered with resuscitation.
Placental transfusion
(PT) filled the lung blood vessels after ventilation and before cord
clamping. PT also filled the gut, the
liver, the kidneys, the skin and the brain with blood.
The PT was clamped in
the baby, not in the placenta. PT
generated very adequate blood pressure and copious tissue perfusion. Placental transfusion prevents
birth brain damage.
Figure 11. The
human equivalent of this monkey is the red baby on the handout.
Handout
Birth Brain Injury and Cord Clamping
No Clamp Used
Immediate Clamping

Normal newborn blood volume Blood volume? Cord pH normal
1882 "Infants
which have had the benefit of late ligation of the cord are red, vigorous, and
active, whereas those in which the cord is tied early are apt to be pale and
apathetic." Lusk WT (1882)
The Science and Art of Midwifery
1801 “Tying
and cutting of the navel string too soon is very injurious to the child; the
child is much weaker than it ought to be, a portion of the blood being left in
the placenta, which ought to have been in the child.” Erasmus Darwin; 1801
1992,1993 Clamping delayed for five minutes
produced routine Apgar scores of 10. Linderkamp ‘1992,1993
1982 “…
immediate cord clamping can cause hypovolemia, hypotension and anemia
…” Linderkamp ‘1982
1981 “Thus [clamping before the first breath] is
unphysiological and should be avoided; under certain unfavourable circumstances
the consequences may be FATAL.” Peltonin 1981
1994-2002 “To obtain a cord pH, doubly
clamp a segment of cord immediately.” ACOG BULLETIN 138
2003
Cowan F …Neonatal Encephalopathy.(NE)
Lancet 2003 Cowan's
clinical definition of NE is:
1. Abnormal tone
pattern Weaker
than it ought to be
2. Feeding
difficulties Not vigorous
3. Altered
alertness Apathetic
4. Late
decelerations Cord
compression in utero
5. Delayed respirations Not
red
6. Arterial cord blood pH >
7.1 Immediate
Cord Clamping to obtain blood
7. Apgar >7 at 5
mins
Pale and apathetic, not active
8. multi-organ
failure Hypovolemic
shock
The clinical definition
of NE is an accurate clinical description of the
immediately clamped newborn. (ICC)
2004 N A Murray. Neonatal transfusion
practice “Sick neonates
(NE, HIE) are one of the most [anemic] heavily transfused
groups of patients in modern medicine.”
1982-2004
Infant anemia correlates strongly
with ADHD, autism, ASD, learning and behavioral
disorders and mental deficiency in grade school
children. Lozoff B. (U.
of M.)
2004 Delayed cord clamping (DCC) prevents brain damage (hemorrhagic
infarction, IVH) and anemia in preterm infants: Cochrane Report. DCC is advocated on term infants to
prevent infant anemia (and childhood mental deficiency:) American Academy
of Pediatrics.
2001-2005 Successful routine prevention of infant anemia,
respiratory distress and HIE by routine cord clamping after delivery
of the placenta. Michigan Midwives Association.
2005 Dec. Green Journal: Experimental attempt to prevent HIE by hypothermia –
cooling newborn brains; editorial and article.
No
informed parental consent
offered for amputation of the functioning placenta.
The mother of the above red infant is not anemic; the red
infant is not at risk for anemia or for hypoxic ischemic encephalopathy;
delivered Jan 14, 2006.
Email obgmmorley@aol.com
This paper
was presented at:
The 5th
International Symposium for the use of Hyperbaric Oxygen in Neurosciences
July 21, 2006, Fort
Lauderdale, Florida